Degenerative disc disease and trauma: the law related to pre-existing conditions
The Law of Pre-Existing Condition and Compensation for Aggravation of Pre-existing Condition
An injured person is entitled to be compensated for any aggravation of a pre-existing condition, but not the pre-existing condition itself. Usually, the aggravation often doesn’t substantially change the physical nature of the pre-existing condition right away, but rather, causes symptoms that require clinical intervention on sometimes multiple levels, including surgery. Because of the physiology of the spine, making the distinction about what symptoms prep-existed a traumatic incident can be confusing.
We are all walking and talking “pre-existing conditions.” Our human flesh, bones, muscles and organs are what they are today, in part, by a long term process of development. Some body parts, such as the spine, naturally change over time physically over time; but often, the person remains without any negative symptoms until a significant trauma occurs. Because of this, defense attorneys, working for insurance companies, create “smoke and mirrors,” suggesting that a person is making a claim for injuries to the neck and/or back were pre-existing, and not related to the most recent trauma. The key factor with neck and back cases is whether the trauma caused the need for clinical intervention.
Attorneys representing people with injuries that are superimposed over a pre-existing condition to the spine should know: (1) the physiology of the spine and how it develops and maintains itself; and (2) the law of pre-existing condition and how a person is entitled to compensation for an aggravation for the pre-existing condition.
The Anatomy of the Spine
Spinal Nerves, Nerve Roots, the Disc (Annulus and the Nucleus Pulposis)
The spinal nerves have nerve roots at the spinal cord. Those roots, including the nerves, can become irritated and impinged upon when there are defects in the spine that come from either the natural degenerative process of the spine, trauma, or a combination of the two. The intervertebral discs serve as cushions between the vertebral bones. On the outside, the disc is made of a “annular” fibers, a strong muscle like tissue that surrounds the “nucleus pulposis.” The nucleus is a gelatinous like material.
When the anullus fibers are torn, the nucleus is often extruded through the annular tear and remains connected to the disc; or it may become a free floating disc fragment. This is a “herniated disc,” a very serious condition an any level of the spine, due to the neurological implications.
Levels of the Spine: Lumbar, Thoracic and Cervical
The spine has three levels, starting at the tailbone, sacrum (Sacroilliac joint), then proceeding upward as follows: Lumbar (Lower back L5S1 to L1); Thoracic (Mid-back T1 to T12); and Cervical (Neck C7 to C1).
Dermatomal Patterns of Nerve Related Pain and Numbness Into Arms and Legs
When the spinal nerves are irritated either at the nerve root, or around the nerve sheath, electrical signals are sent through the nerves into the corresponding arms or legs. This is why, after an injury in an auto wreck, or other kind of traumatic incident, people often experience pain and numbness into one or more of their extremities. Doctors refer to this as “radiculopathy,” or radicular” symptoms. This nerve related pain can indicate either that there has been some muscle tissue swelling that is causing some irritation, or there could be some disc involvement; or a free fragment, part of the nucleus pulposis that has come outside of the ruptured, herniated disc and is “floating” around and impinging the nerve. The neurological symptoms can be related to irritation from bone itself.
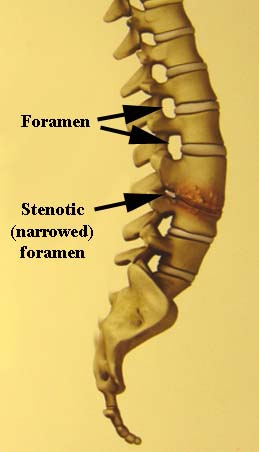
Foraminal Stenosis (Narrowing of Foraminal Canals)
The nerves run from the spinal cord through small holes in the vertebra called foramina, or foramnal canals. Sometimes these foraminal canals will have calcium build up over time, called “ossification” and other bone spurring in and around these nerve canals. After a trauma, because the canals were already slightly narrowed and compromised, a person is more likely to become symptomatic following a trauma, than a person with a completely healthy spine. However, people with narrowing of the foramina, in the absence of trauma, often feel no symptoms whatsoever. Here is an illustration of severe narrowing of the foraminal canal.
Degenerative Disc Disease
The Southeastern Spine Institute in Charleston, SC, describes the process of degenerative disc disease as follows:
- THE DISC WALL TEARS
As shown in illustration 1, degenerative disc disease usually begins when small tears appear in the disc wall, called the annulus. These tears can cause some pain.
- THE DISC WALL HEALS
The tears heal, often in a matter of weeks, but the healing process creates scar tissue that’s not as strong as the original disc wall. See illustration 2. If you keep injuring your back, the process of tearing and scarring can continue, which further weakens the disc wall.
- THE DISC CENTER WEAKENS
Over time, the nucleus or center of the disc, called the pulposus, becomes damaged, losing some of its water content. The pulposus needs its water content to keep the disc functioning properly as a shock absorber for the spine. Refer to illustration 3.
- THE NUCLEUS COLLAPSES
As shown in illustration 4, if the disc can no longer act as a cushion, the nucleus collapses. The vertebrae above and below this damaged disc slide closer together. This improper alignment causes the facet joints — the areas where the vertebral bones touch — to twist into an unnatural position.
- BONE SPURS FORM
In time, this awkward positioning of the vertebrae may create bone spurs, as shown in illustration 5. If these spurs grow into the spinal canal, they can pinch your spinal cord and nerves, a condition called spinal stenosis.
These “injuries” referred to can be small micro-tears that cause little to no pain, injuries related to every day activities. But then once compromised, a more significant trauma can be the straw breaker and cause a disc rupture, or cause a previously asymptomatic disc and surrounding nerve roots to become painful, with nerve involved pain and numbness into the extremities. Therefore, it is not uncommon for patients reporting a history of no pain, to be in an auto accident, or other trauma, have pain following it, then be told that what is shown on an MRI is a lot of old injuries. It leaves people perplexed as to how they had old injuries, and a “chronic condition” going on pre-accident, but they never felt anything, and never saw a need for clinical intervention.
The MRI and CT Scans Don’t Tell the Whole Story
It is important to point out that most people over the age of 35 will be said to have degenerative Disc Disease, because it is part of the natural human condition, with all spines prone to degeneration over time. However, the scope of the degeneration and the speed at which the degeneration occurs varies from person to person; and as stated above, there is not always a correlation between the physical findings and symptoms and the need for clinical intervention.
There are people who are diagnosed with severe degenerative disc disease, who accurately and truthfully report no symptoms of pain or numbness or other nerve related sensation. There are people whose diagnostic studies, MRI and CT scans, show very little degenerative disc disease, who report symptoms of pain. The fact that a person has narrowing of the foraminal canals, or degenerative disc disease, is no indicator as to whether the person is having symptoms, unless it is severe with definite nerve root impingement.
A Person’s History of Doctor’s Visits or other Clinical Intervention is a Strong Indicator of Past Symptoms or the Lack Thereof
A patient who presents with back or neck pain, who may also have extremity pain or numbness, and who reports never having this frequency or intensity of pain prior to the subject trauma in question, is normal and reasonable, given the natural, often asymptomatic degenerative process that goes on with the spine. A trauma on top of a non-symptomatic spine that is going through the natural process of aging, can turn a completely healthy feeling person into an out of control, painful person. Then, to have to argue with an insurance company or insurance defense lawyer, and spend thousands of dollars on litigation and expert testimony to prove medical causation, is a frustrating experience for many.
Hired Gun “Expert” Witness Doctors say all Injuries are Old and Pre-existing Injuries
It is common in cases involving injuries to the back or neck for insurance companies and their lawyers to have “hired gun” expert witness doctors, who make a living testifying for insurance company lawyers, conduct a records review and testify that all of the problems complained of are old, pre-existing problems, and that all of the pain and clinical intervention following a trauma in an auto or other traumatic accident pre-existed the accident and is simply part of the “natural progression” of the degenerative process of the neck or back.
Conclusion
The diagnostic studies such as MRI, CT scans and x-rays only tell part of the story; because even though the spine naturally goes through degenerative changes, those changes are often pain free. Only when a trauma aggravates the non-symptomatic pre-existing degenerative changes is there any pain or other symptoms that require clinical intervention.
Legal counsel with a thorough knowledge of the science of the spine and experience in cross-examining “expert” insurance company “experts” is crucial to getting to the truth. Also, the attorney must know all the right questions to ask the patient’s treating physician, so that he or she can make these distinctions and show that even though this “chronic condition” of the spine probably pre-existed the trauma, it is scientifically reasonable that it was non-symptomatic, and reasonable that without the subject trauma, it would have remained that way for an indefinite period of time; and that the therapy, injections and other more significant clinical intervention, such as surgery, including future care, is directly a result of the subject trauma.
This brief article only touches on the physiology of the spine and the medical/legal causation issues that lawyers face in proving that the clinical intervention of a patient/client was caused by the trauma, and that the known pre-existing chronic condition was not symptomatic prior to a traumatic incident. It is a complicated scientific analysis that must be understood for effective cross examination of insurance defense “hired gun” experts. Further, one must understand not only the pre-existing condition issues related to the spine; but also, the science underlying the fact that after trauma, arthritis/degeneration of the neck and back discs tends to accelerate, leading to reasonably forseeable medical care into the future. We can save those issues for another article.
Contact Charleston accident attorney Jody McKnight with questions, or for a case consultation.